Just a spoonful of sugar
Claire Morrow wonders why placebos sometimes work better than nothing
Penicillin paediatric syrup is, to my mind, one of the most therapeutic possible smells. The white one, not the orange one. They’re the exact same thing, of course, I just happen to associate one of them with getting better; that was the stuff you got when you were really sick and then you got better. That sweet white medicine must work. Oh, and soluble aspirin, the sweet, fizzy kind. I am loathe to this day to take non dissolving aspirin.
The other stuff simply doesn’t work as well, even though it is the exact same medicine, and I know perfectly well that it does work exactly as well. Except, of course, that it doesn’t. Maybe.
The Placebo effect was described in detail in a 1955 medical paper called The Powerful Placebo, and changed the way medicines and other treatments are assessed. When a drug company makes a medicine it must prove that it (relatively) safe and that it works. But just giving a group of patients medicine and seeing if they get better is not enough. Maybe they were going to get better anyway. Maybe they got better because they saw the clinic nurse every day, and they benefitted from her smile and the walk to the clinic, and so forth. And so we have the idea of the randomized, double blind placebo controlled clinical trial. Now we have (at least) two groups of patients, randomly divided into two groups: those who receive treatment, and those who receive a fake treatment, which in all accounts is identical to the real one. No-one knows which patients are receiving the real treatment, and which are getting the dummy, the code isn’t broken until the end of the trial. To be worthwhile, a new treatment must do better than the placebo treatment. It is very common for the placebo treatment to be fairly effective, more effective than no treatment at all. But why?
Many symptoms, like pain and depression, really are amenable to circumstance. It’s not that your pain is all in your head (in the sense that it’s made up), but it’s certainly modified by circumstances. The headache doesn’t seem so bad if you’re distracted, the toothache is tolerable since you’re in such a good mood. The expectation that things which taste of sweet fizzy aspirin make headaches better is likely to make headaches remit with the administration of sweet fizzy things. But that’s not all there is to it.
Telling someone they will feel better (or worse) if they take tablet X is likely to cause it to have that effect, if they believe you. But telling someone that injection X will increase their secretion of growth hormone doesn’t increase their secretion of growth hormone. However, giving an injection that has this effect, then swapping it for an identical (but inactive) injection allows the inactive (placebo) medicine to work. And it still works, even when the patient is told it will have the opposite effect. This is, of course, quite involuntary. The brain has been taught to do something when it gets an injection, and it intends to do it. Imagine teaching a dog to sit, then trying to teach it to ignore the command, just when it’s got the idea of what it should do.
So something really is happening with placebo effects. Recent research has shown that people who respond to placebo painkillers and antidepressants are not just pulling their socks up because the doctor was nice to them. For people who get a strong positive response to their placebo treatment, they are not getting “no treatment”. Their brains are changing their chemicals (not activating the pain sensors, or releasing endorphins, or pumping out the naturally occurring chemicals that relieve pain, or lighten mood). Dopamine, for example, is used to treat Parkinson’s Disease, amongst other things. In patients who respond to placebo treatment, they really are feeling better, because their brain really is producing more dopamine.
Not all maladies respond to placebos, and not all people do either (nor do all people respond to every medicine, of course). And conditioning is significant. A drug can perform much better than placebos in one country, and worse in another, due to local beliefs about the likely efficacy of treatment. When antidepressants first came out, they seemed to work much better than placebos. They now don’t. They work as well as they ever did, but placebos get a much better response. Presumably seeping cultural belief that pills relieve depression makes trial subjects more susceptible to getting better. In fact, the two are about equal (you are as likely to get well on sugar pills as on antidepressants), but there seems to be some difference – recent research suggests that it’s possible to predict which patients will respond to placebo and which won’t based on their brain chemistry.
Primo Non Nocere, meaning “First Do No Harm”, is often cited in defence of placebos. They can’t hurt and may make you feel better. Unlike “real” medicine, which can hurt you and may make you feel better. But I am not sure. Placebo surgery (put the patient under, make an incision, do nothing useful) is effective for some things, but there is surely some risk involved with the anaesthetic and the theatre, and the cost. Believing in medicine which doesn’t work means taking medicine which doesn’t work. It enforces an idea that one should always take a tablet if they feel sick. I remain divided on the topic.
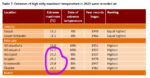
And as to the fizzy aspirin? As far as placebos go, unconscious cultural conditioning is important. In our part of the world the most effective placebos are the more expensive ones; brand name placebos work better than generic looking placebos, more costly placebos are more effective.
More pills work better than less pills, capsules work better than tablets, and colour is important. Yellow placebos are better for depression, blue placebos are better for sedatives. But in Chinese medicine, there is a saying that “no-one trusts pleasant tasting medicine”. It may be all in your mind, of course, but then, the mind is an incredible thing.